Maternal Vaccination Series Part 1: The Birth of Maternal Vaccination
How a standard of care practice came to be.
Anti-vaccine propaganda targets parents overwhelmingly, as they are typically the ones making decisions about whether or not a vaccine should be given. Pregnancy is often a particularly anxious time: many of the things perfectly fine to do outside of pregnancy suddenly become unacceptably risky. People sacrifice a lot of personal comfort, sometimes even undertaking significant personal risks with their health, for the promise of a healthy child. It’s a lot of pressure and it’s a situation that makes it easy to be misled. It’s very easy to scare people- it is much harder to un-scare them. Here, I begin a series all about maternal vaccination which will cover everything including the history of maternal vaccination, the mechanisms behind it, safety considerations specific to maternal vaccination, vaccines and vaccine-preventable diseases of special importance in maternal vaccination, and future maternal vaccines to look forward to. In this first post, I deal with the history of the practice of maternal vaccination.
Today, in the US, 4 vaccines are routinely recommended in pregnancy (and many, but not all, additional vaccines can be given if needed depending on individual circumstances):
Influenza (at any point in the pregnancy, dictated by the spread of flu, in every pregnancy)
COVID-19 (at any point in pregnancy, dictated by the spread of SARS-CoV-2, in every pregnancy)
Tdap (to protect against tetanus, diphtheria, and pertussis, given in the third trimester of every pregnancy)
Pfizer’s RSV vaccine aka Abrysvo (between 32 and 36 weeks gestation, unless the infant will receive the RSV monoclonal antibody nirsevimab after birth if there aren’t additional risk factors; currently only given once but this may change as we learn more about the antibody response to the vaccine over time)
These recommendations didn’t just poof into existence- how did we get to this point?
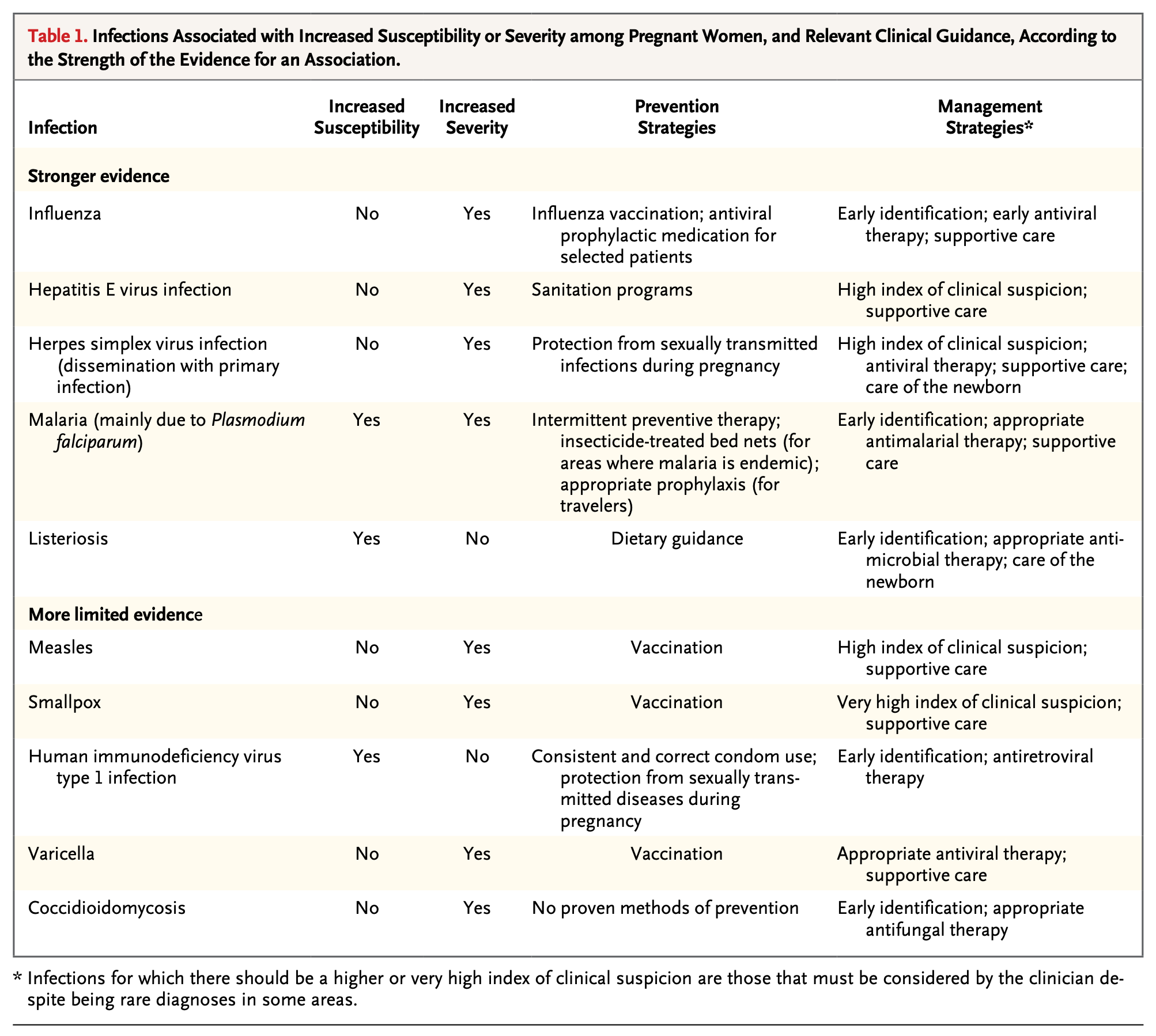
The practice of maternal vaccination has an extensive history comparable in its scope to that of the history of vaccination as a practice. It was borne out of a basic observation: many infectious diseases tend to be more dangerous in pregnancy1:
Measles was noted to be more severe in pregnancy as early as in the 1840s by Panum in his famous trip to the Faroe Islands2. The mortality from influenza during the 1918 pandemic was drastically higher among pregnant individuals compared with their non-pregnant counterparts (27% vs. ~2%)- a finding first noted as early as 1919. Smallpox vaccination had been done in pregnancy since the 1800s, and, in 1879, Burkhardt observed that infants born to mothers vaccinated with the smallpox vaccine seemed to be resistant to developing smallpox. Reports from the 1800s also noted that pregnant individuals receiving smallpox vaccines had at least partial protection from the disease3. By 1895, it had been noted that antibodies to diphtheria toxin were present in the umbilical cord, and as knowledge of passive immunity expanded in the 20th century, it was noted that the immunological history of mothers (the record of the infections they encountered as chronicled in the form of antibodies) could translate into protection for their infants.
Trials of the Diphtheria-Tetanus-Pertussis (DTP) whole cell vaccine were carried out during pregnancy, with the first clinical evidence supporting its use seen as early as 1938, although it had been noted that vaccinating pregnant rabbits resulted in the transfer of antibodies to their offspring in 1935. As early as the 1950s and 1960s, vaccination of pregnant individuals with influenza and polio vaccines was carried out as a routine part of their care to both protect them and their infants.
It became apparent however that some infectious diseases were uniquely dangerous for the fetus, even if they weren’t anything special for the pregnant person. The first of these was rubella (also known as German measles, but not to be confused with measles itself), in 1941, when Australian ophthalmologist Norman Gregg linked rubella infections in pregnancy to cataracts in children. His findings were initially met with skepticism, but confirmed shortly thereafter, and knowledge of the devastating effects of rubella when contracted in the first trimester became undeniable when an epidemic in the 1960s resulted in 30,000 spontaneous and induced abortions from rubella-associated congenital anomalies in the US. The list of these infections grew over time into what is sometimes known as the TORCH complex4- a group of infections that can be transmitted from the pregnant individual to the fetus via the uterus and inflict catastrophic harm upon the fetus. Efforts to make a rubella vaccine were undertaken and eventually a vaccine was made- but there was an issue. The vaccine involved a live rubella virus that had been adapted to be ineffective in causing disease, but the theoretical risk existed that it could infect the fetus and cause congenital rubella syndrome5. Thus the vaccine had to be given to everyone except pregnant people, with great success: rubella was declared eliminated6 from the US in 2004 and as of 8 July 2020, 84 of 195 (43%) countries have eliminated rubella, a testament to the power of herd immunity.
Another disease however was determined not to be forgotten. The incidence of pertussis had been steadily increasing since about the 1980s (for reasons that are too complex to get into here for reasons of length- they will be covered in the post specifically about maternal pertussis vaccination), and things came to a head in 2005 with a dramatic resurgence. Cases eventually began to accumulate in infants too young to be vaccinated with devastating consequences, at which point the US CDC, in 2010, recommended a maternal dose of pertussis vaccine. They updated the recommendation to include a booster dose with every pregnancy shortly thereafter.
Most recently, pregnancy was observed to be a major risk factor for severe COVID-19 and poor pregnancy-related outcomes, although there is some disagreement across studies regarding certain risks (specifically stillbirth- although the evidence that this is a risk for infection by the Delta variant is, in my view, quite convincing; the extent to which it holds true of other variants is less clear). In fact, COVID-19 directly contributed to a huge rise in maternal mortality in the US:
Given these observations, the recommendation to vaccinate against COVID-19 during pregnancy was made by multiple expert bodies across the world. Some have incorrectly argued that this recommendation was made despite the complete absence of data on COVID-19 vaccination in pregnancy, and more puzzlingly still, some claim we still do not have the data to justify the use of COVID-19 vaccines in pregnancy. Neither point is correct. Firstly, we did have developmental and reproductive toxicity studies (DART) on rodents with the vaccines that did not flag any unique safety concerns, but we also did have pregnant individuals in the COVID-19 vaccine trials (these pregnancies were accidental)- outcomes were similar across vaccine and placebo groups. We have however rapidly accumulated data on hundreds of thousands of pregnant individuals who received COVID-19 vaccination and the findings are extremely reassuring regarding their safety and the value added to the infant as far as protection from COVID-19.
The most recent update came with the maternal RSV vaccine. RSV is the leading cause of hospitalization in infants and we have tried for a vaccine since the 1960s. Unfortunately, progress was greatly hampered with the failure of the Lot 100 vaccine (details in the hyperlinked post), and it was not until very recently that an RSV vaccine meeting standards of safety and effectiveness could be approved. Because RSV is especially dangerous for the youngest infants, vaccination in pregnancy is the obvious answer. However, on the heels of the RSV vaccine’s success, a monoclonal antibody (nirsevimab) has been developed that also protects very well against RSV for many months. The problem here however is that supply of this monoclonal is very limited and the manufacturer (Sanofi) was apparently unprepared for the broad recommendation given for its use, causing substantial shortages and lack of coverage. Navigating RSV vaccination for infants will be the subject of a future post.
In sum, we’ve covered how we got to the current recommendations for maternal vaccination by tracing the history of the field and how it responded to new developments across infectious disease epidemiology and medicine.
The next post in this series deals with how maternal vaccination protects infants.
I promise to discuss this in greater detail in a future post, but it should be noted that while often taught that pregnancy is an immunocompromised state as a consequence of the need for the pregnant individual to not reject the fetus, this viewpoint is considered outdated and not consistent with the totality of evidence. The immune system undergoes many changes in pregnancy (as does the rest of the body), which may increase the risk of some infectious diseases, but it is misleading to describe pregnancy as an immunocompromised state.
Panum’s trip to the Faroe Islands is famous within the field of infectious disease epidemiology because it was one of the earliest field observations of the ability of immunological memory to protect people from re-exposure to a microbe and it established the essentially permanent protection elicited by measles infection against measles reinfection (of course, assuming you survived it). The Faroe Islands reprised a role in the history of infectious disease epidemiology during the COVID-19 pandemic, wherein they were the site of one of the first superspreading events of the Omicron variant among highly vaccinated people, and thus one of the first indicators that Omicron was very good at evading antibodies elicited by the vaccines.
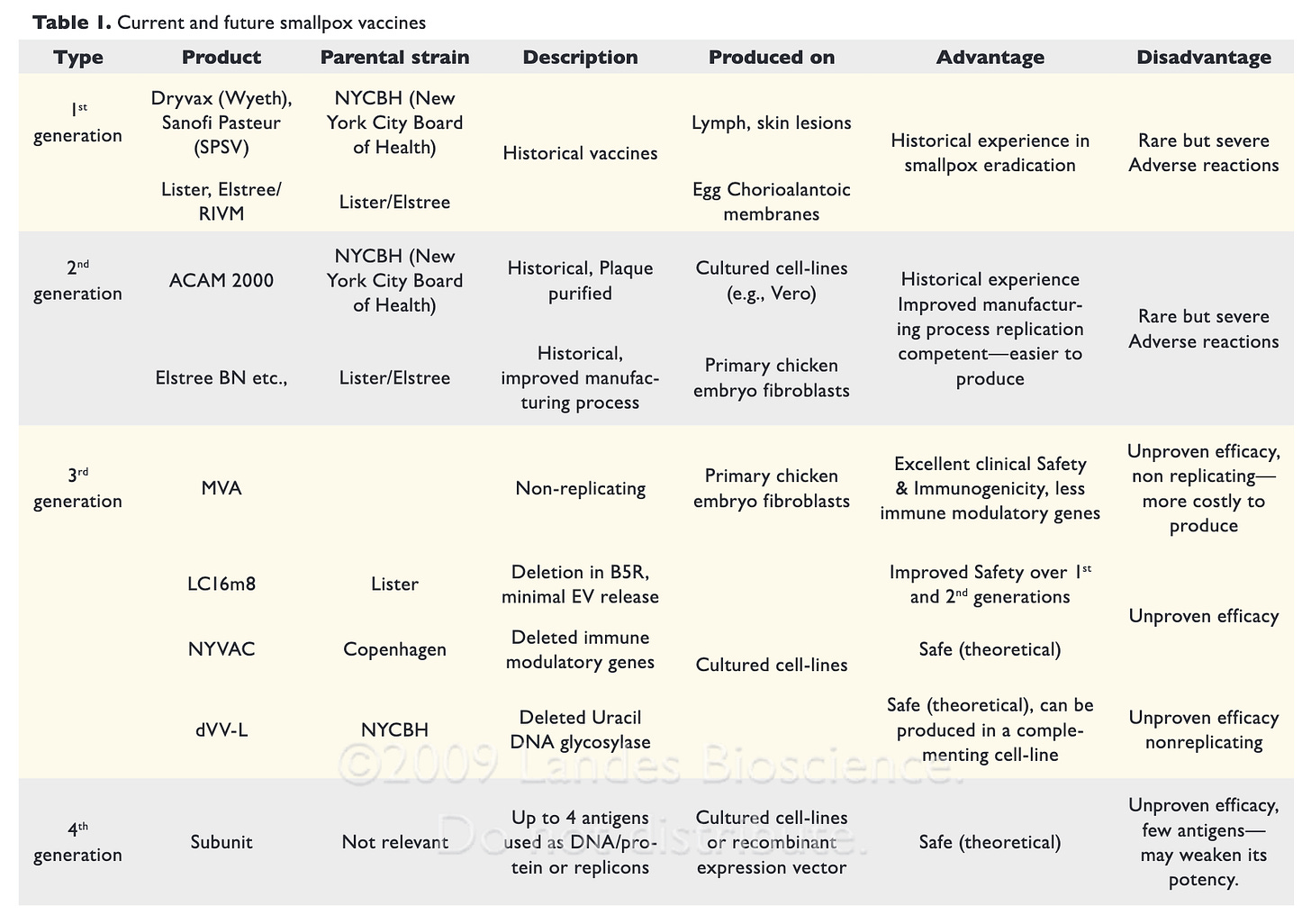
We are fortunate enough to live in a world where smallpox virus (variola virus, VARV) has been eradicated- although its orthopoxvirus relatives like mpox are still very much around. Because of this, we do not have to carry out smallpox vaccination routinely, especially during pregnancy. Smallpox vaccines are fairly unique in terms of their safety profile as vaccines- the first- and second-generation vaccines tend to have much higher risks than any vaccine used routinely (which is considered acceptable only because smallpox is so dangerous and because we no longer use them routinely):
For this reason, any kind of smallpox vaccination today involving pregnant or lactating individuals would almost require exposure to VARV or a related orthopoxvirus to justify. However, in an era where VARV was very much around, it is understandable that the risks of the older generation vaccines might be acceptable even in pregnancy.
TORCH is an acronym for Toxoplasma gondii, Other (Treponema pallidum pallidum- the causative agent of syphilis, hepatitis B virus), Rubella, Cytomegalovirus, and herpes simplex virus, but the acronym has been criticized for not being comprehensive enough. Another version, CHEAP TORCHES, attempts to be more comprehensive by including chickenpox (varicella zoster virus), HIV, hepatitis C virus, hepatitis E virus, enterovirus, parvovirus, lymphocytic choriomeningitis virus, malaria, tuberculosis, etc. There has been debate about whether or not SARS-CoV-2 should be considered a TORCH pathogen; while pregnancy absolutely is a risk factor for more severe COVID-19, at present, there is (thankfully) not any obvious increase in the incidence of congenital anomalies to children born to those who become infected with SARS-CoV-2 during pregnancy. It should be noted, however, as discussed above, that SARS-CoV-2 (particularly the Delta variant) was shown to potentiate catastrophic outcomes in the fetus through infection of the placenta even in cases where infection was apparently mild- but in all documented cases of placentitis resulting in stillbirth, the pregnant individual was unvaccinated.
This risk has been a focal point of safety considerations with maternal vaccination; in general, live attenuated vaccines are not permitted in pregnancy on this basis (but there are exceptions). Rubella is most dangerous in the first trimester, and at this point, many people may not know they are pregnant, so many pregnant individuals have received rubella vaccinations (mainly in the form of MMR) inadvertently or through immunization errors. Hundreds of such vaccinations are documented and there has been just 1 case of congenital rubella syndrome observed from the vaccine strain in the entire time of the vaccine’s use.
The term “elimination” is an important one in infectious disease epidemiology and it is often confused with the term “eradication.” To clarify:
Control: The reduction of disease incidence, prevalence, morbidity or mortality to a locally acceptable level as a result of deliberate efforts; continued intervention measures are required to maintain the reduction. Example: diarrhoeal diseases.
Elimination of disease: Reduction to zero of the incidence of a specified disease in a defined geographical area as a result of deliberate efforts; continued intervention measures are required. Example: neonatal tetanus.
Elimination of infections: Reduction to zero of the incidence of infection caused by a specific agent in a defined geographical area as a result of deliberate efforts; continued measures to prevent re-establishment of transmission are required. Example: measles, poliomyelitis.
Eradication: Permanent reduction to zero of the worldwide incidence of infection caused by a specific agent as a result of deliberate efforts; intervention measures are no longer needed. Example: smallpox.
Extinction: The specific infectious agent no longer exists in nature or in the laboratory. Example: none.
A disease can be considered eliminated from some place but cases may still occur so long as they are imported and transmission is not sustained.