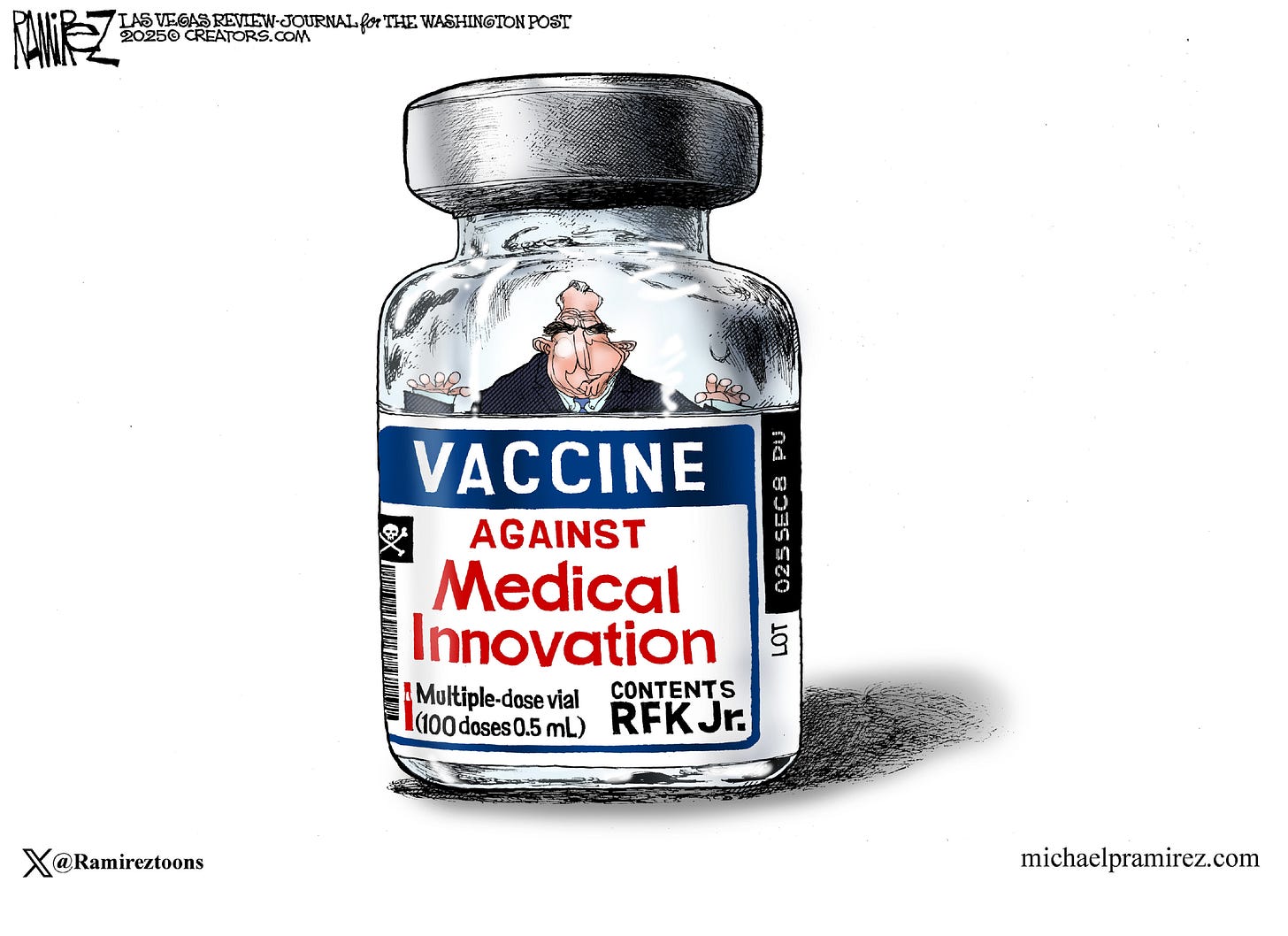
HHS and FDA Demand Unethical Vaccine Studies
RFK Jr's. HHS is attempting to demand placebo-controlled trials in cases where it's not ethically appropriate.
The Washington Post recently broke the story that HHS, under the leadership of Secretary Robert F. Kennedy Jr., will be demanding that all new vaccines complete placebo-controlled trials before licensure. HHS’s comments therein note that Kennedy is not anti-vaccine, but rather “pro-safety”- a bald-faced lie that insults everyone’s intelligence. Similarly, FDA Commissioner Makary seems to be pushing for Novavax to conduct a randomized efficacy trial of their COVID-19 vaccine under the claims that it is a novel product because it has changed the strain of the spike protein it uses (it is not a novel product under existing regulatory framework and simply by common sense). I understand that headlines on this question have sparked confusion (e.g., “RFK Jr. will order placebo testing for new vaccines, alarming health experts”) and it may not be immediately clear why the health experts are alarmed. Here’s my best attempt to explain:
Some hypotheticals for you to consider
Over on Threads, Dr. David Higgins offered the following thought experiments to illustrate the problem with HHS’s demand:
✅ New car seat? Randomize some infants to the new design and some to nothing at all (placebo) to see which is most effective and safe.
✅ Updated antibiotics? Half the patients get the new drug. The rest get sugar pills.
✅ Improved life jacket? Half the boat gets them. The other half gets a recommendation to swim.
✅ Newer bike helmet? Send half the kids down the hill without.
✅ New parachute design? Half jump with it… you get the point.
As described, any and all of these trials would represent major ethical breaches that should have (and barring unbelievable process failures absolutely would have) been caught by the Institutional Review Board (IRB), the Office of Human Research protections (OHRP), and frankly the investigators and sponsors proposing the study1. You are effectively sentencing whoever ends up in your control group to grievous harm if not death despite the availability of an effective intervention(s) to protect them.
You cannot withhold a standard of care treatment when one exists simply to see whether or not the experimental treatment works. You cannot regard human life, nor quality of life, to be a disposable quantity simply because you think it makes it easier to gather data (which, by the way, if you do think that- skill issue on your part). This is not up for debate- it is written in the blood of the victims of medicalized torture attempting to be passed off as clinical research. If you do not respect the value of human life, there is no place for you in clinical research- and actions speak much louder than words here.
Let’s apply this to vaccines for a moment.
Jonas Salk strenuously objected to the use of a placebo in his trials of the polio vaccine because he knew it meant some children would be paralyzed when they could have been protected- and he was right2. Polio is not the only scary vaccine-preventable disease, however. Imagine children with muscle spasms locking their back in an arched position, forced into a smile they do not mean, with their diaphragm’s locked in contraction unable to breathe. Or children visited by diphtheria, the strangling angel as it was known then, as a thick, gray membrane coated their throat until they suffocated. Or babies coughing so hard from pertussis that they develop brain damage from the lack of oxygen. Or adolescents slipping into irreversible coma and dying from subacute sclerosing encephalitis caused by a measles infection years earlier. These are not theoretical, hypothetical risks. They are the uncaring, vicious reality of the evolutionary imperatives of pathogens: to spread as much as possible.
So, when can we use a placebo?

This is the critical question and it is thoroughly discussed in these recommendations.
In general, all new vaccines (that is, first-generation vaccines) use a placebo control for their prelicensure evaluation. Past the first-generation, many vaccine trials do not use an "inert" placebo (i.e., sterile saline) as the control. Placebos are principally useful for the evaluation of the efficacy of a treatment, but they are not absolutely required. As discussed earlier, for placebos to be used, there must not be an existing standard of care intervention (with some specific exceptions- explained shortly).
Placebo use is justifiable for first-generation vaccines because at the point of evaluation, safety and efficacy of the product are not known, and the history of vaccines demonstrates that in addition to a mere failure to protect against the outcome in question, there are instances where exposure to a vaccine may worsen disease (e.g., killed measles vaccinees developing atypical measles upon challenge, Lot 100 RSV vaccine, Dengue and antibody-dependent enhancement, etc.). This means that the condition of equipoise (there is genuine uncertainty about the relative balance of benefits and harms for the vaccine) is met and the use of placebo is justified. So long as this is unknown for the new vaccine, the condition of equipoise is met, meaning a placebo is ethically appropriate. However, once a first-generation vaccine has already been approved, it has been deemed to have met a bar of safety and efficacy that is acceptable for its use. Note that this does not mean that the vaccine is either completely safe (i.e., has no chance of causing any adverse effects at all) or completely effective (i.e., it creates a magic forcefield around you that renders you uninfectable)- this is not the standard applied for literally anything. Everything we do has risk. We weigh those risks against the benefits to come to a choice about how to act.
To study a next-generation vaccine and compare it with placebo would mean that you would be withholding the protection of the previous-generation vaccine from your trial participants, which is a major breach in the ethical and legal obligation to protect clinical trial participants as much as possible.
Furthermore, in terms of the quality of the science being done, the value of a second-generation vaccine is based on whether or not it meaningfully adds to the current armamentarium of protection against the infectious disease in question. The most direct way to gain insight into this question is through the use of the first-generation (or previous-generation) vaccine as the control.
At times, other controls may be used as well. For example, because the protection elicited by vaccines absolutely requires the presence of the immunogen, preparations containing everything in the vaccine except for the immunogen can be valuable in that they will often reproduce the local and systemic reactogenicity from the vaccine to preserve blinding. In some cases, a vaccine against a different disease may be used for the same reason.
In addition to the blinding aspect, in some instances, nonspecific protection by some vaccines has been observed as a consequence of exposure to the adjuvants or the off-target vaccine, which further enhances the protection extended to clinical trial participants. The corollary to the objection about placebo use (or lack thereof) in vaccine trials is that employing other controls masks potential safety problems with the vaccines during the clinical trial process. This is inaccurate.
Firstly, though clinical trials for vaccines are frequently very large (potentially enrolling tens of thousands of individuals), regardless of placebo use, it is not possible to capture extremely rare adverse events (e.g., intussusception with the Rotashield vaccine for rotavirus- 1 excess case in 10,000 doses), meaning that post-marketing surveillance is required.
This allows for examination of far larger numbers of individuals to determine an excess risk or lack thereof for a given adverse event and the study designs involved for such pharmacovigilance are much more suitable for this analysis than are RCTs if only because of their size. Additionally, even if the comparison is made to a prior generation vaccine or a different vaccine, the safety profile of those vaccines is well established with the combination of prior clinical studies and post-marketing surveillance data. Excess risks of adverse events can still be observed and inform safety considerations. When adverse events occur that are not in excess relative to the comparator, it suggests that there is not a substantial difference in their frequency- and we have already judged the comparator products to have met an acceptable margin of safety for use.
There are some cases where a placebo may be appropriate despite it initially seeming that it might not be, and some cases where a placebo would be inappropriate in cases where it seems like it should be in the context of vaccines. One instance is when evaluating the effectiveness of a vaccine in a local context when we lack insight into how well the vaccine works in that area. Specifically, because we know that microbes have different strains which vary in their ability to resist the protection conferred by vaccine-elicited immunity, the use of a placebo may be justified when considering the effectiveness or efficacy of a vaccine in a specific region when there is a lack of data to inform how it works in a local context, even if that data exists elsewhere. For example, there are over 100 distinct strains of pneumococcus (Streptococcus pneunmoniae) which can cause devastating infections across many demographics, including young children. We have vaccines targeting a subset of these strains (up to 21), but the specific strains causing disease in parts of the world may vary. To assess how a vaccine based on the predominant disease-causing strains works in e.g., Canada, it may be reasonable to use a placebo comparator.
Where are the placebo-controlled vaccine trials?
These can be harder to track down for vaccines that first came out many decades ago because of the differences in publishing practices. The easiest way to find the data for a given vaccine is to look at the FDA new product license applications; some of these may be archived. Another option is to use Pubmed. For example, this search identifies vaccine trials using a placebo, which can be narrowed to look for a specific vaccine (you should try not to use the brand name of the vaccine if you do this looking for pre-licensure trials). Some are working on compiling a repository of these trials- I may update this post with a link to one.
Which vaccines could be in trouble from these requirements?
The immediate ones that stand out are the COVID-19 vaccines. Under the current regulatory standards, COVID-19 vaccines are all considered one product despite the updates to strains that occur seasonally to keep up with the evolution of the virus, just as is the case for flu vaccines. This means that when a vaccine is updated, there is no need for a clinical trial to be conducted to prove that the strain updated vaccine is safe and efficacious yet again- those trials have already been completed.
It has been implied by some that this approach is used to save pharmaceutical companies money so that they don’t have to pay for clinical trials, but this is a remarkably shortsighted argument. Even today with the extremely rapid ability of vaccine manufacturers to pivot strains as they emerge, the process of updating a strain and manufacturing the new vaccine in the quantities needed for effective public health campaigns takes months. During that period, SARS-CoV-2 is not pausing its evolution while we get ready- it can undergo another leap in its evolution so that by the time a clinical efficacy trial is completed with the updated strain, that strain of vaccine is now obsolete. This issue most recently became the focal point of the approval of Novavax’s COVID-19 vaccine, with comments from FDA officials being unclear about whether the clinical trial in question would be a post-marketing agreement or a condition for licensure. HHS and FDA have suggested that flu vaccines are exempt from this because of decades of experience with the platform, but this is a tenuous argument and difficult to take at face value.
The underpinning of this claim is in the fact that the COVID-19 vaccines in question are licensed (or about to be licensed) on the basis of trial completed years ago, and so we don’t actually know how well the vaccines work- but this is incorrect. In fact, we do collect data on how well the vaccines perform across multiple networks using a test-negative design, which is generally regarded as the gold ideal study type for vaccines against influenza and SARS-CoV-2.
If we delay approval of updated vaccines because HHS and FDA want to ignore the very carefully considered regulatory basis of the update process, we could be jeopardizing the health of millions of Americans. I also wouldn’t count on the flu vaccine updates being exempt from this.
What should vaccine trials measure?
In most cases, the endpoint (the thing the trial is designed to measure) for clinical studies of vaccines are based on the evidence of clinical disease and efficacy is measured by comparing the incidence of the outcome of interest in the vaccine vs. control group. In some cases, this type of design is impractical or infeasible.
For example, some infectious diseases are so dangerous that a trial that would involve exposure of human subjects to the agent in question, even through natural introduction, would be too risky. In this very unique case, the FDA's Animal Rule may be invoked wherein the vaccine attains licensure on the basis of animal studies. This is strictly a last resort pathway to licensure when no other options are suitable and is the pathway by which the Biothrax anthrax vaccine was approved.
In other instances, the epidemiology of the infectious disease in question may not be amenable to the standard field study, such as is the case with Chikungunya, which typically has extremely rapid, massive, and unpredictable epidemics that render a standard efficacy assessment infeasible, and so the live attenuated chikungunya vaccine Ixchiq was licensed based on immunogenicity endpoints (i.e., how well it triggered an immune response that was shown to be protective in monkeys).
Another potential problem that may arise is that the infectious disease in question is too rare in the setting in question for a field trial, in which case controlled human challenge studies may be done, as was the case for the cholera vaccine Vaxchora.

In the event that there is a well-established immunogenicity signature that is strongly associated with protection (known as a correlate of protection), vaccines may be approved under immunogenicity endpoints. This approach is frequently applied when extending use of a vaccine to an age group it was not initially licensed for use in, and is known as immunobridging. The use of correlates of protection to inform licensure of a vaccine product is an excellent way to protect clinical trial participants because it does not require them to risk the consequences of an infectious disease to learn about whether or not it the vaccine works and should be used in a given group. There are important limitations to the immunobridging approach, but they are beyond the scope of this current discussion.
All of the approaches we have for evaluating vaccines are carefully calibrated to minimize risk to the clinical trial participants who are selflessly working to advance the human condition and give us all the information we need to evaluate how best to use new vaccines. Demanding a placebo-controlled trial in all cases is the sort of thing that sounds superficially appealing, but ultimately puts clinical trial participants at risk and represents an assault on inviolable ethical and legal principles that have been enshrined in the blood of those who bore the weight of the atrocities that gave rise to these guidelines.
The ethical framework for clinical research has, as one of its most critical considerations, the safety and wellbeing of clinical research participants. This is made absolutely clear in the FDA’s Common Rule, The International Council for Harmonization (ICH) Guidelines on Choice of Control Group and Related Issues in Clinical Trials, Council for International Organizations of Medical Sciences (CIOMS) and WHO International Ethical Guidelines for Health-related Research Involving Humans, and many more documents that form the central ethos of clinical research. Those interested in a more detailed discussion of the relevant ethical principles and critical documents that establish these principles may find the Oxford Textbook of Clinical Research Ethics) instructive.
It should be noted that though Salk’s ethical objections to the use of placebo are very understandable, from the perspective of clinical research ethics they do not hold water. At the time of the trials, there was no standard of care intervention to prevent paralytic polio, and we had no evidence that Salk’s vaccines worked (this was the point of these trials). If Salk’s vaccine did not work, or, worse, if Salk’s vaccines increased the risk of polio, then it would not be appropriate to use the vaccines for the public, and in the end, the placebo group would have likely been better off- not having them would have resulted in a greater risk to the clinical trial participants overall. In clinical ethics, this state is known as equipoise- there is genuine uncertainty about whether or not a treatment is effective and so a trial must be done to resolve that uncertainty. Equipoise is one of the major conditions required to justify a clinical trial.





My cat is constantly testing the theory of gravity. At least he's having fun doing it.