Are there racial differences in the function of the immune system?
A critical look at a claim made by Robert F. Kennedy Jr. during his Senate HELP Committee hearing.
During the Senate HELP Committee hearing for Robert F. Kennedy Jr’s nomination for HHS Secretary, Kennedy made a remark that black people were shown by Poland to have “better” immune systems and so black people may benefit from a schedule with fewer antigens. A point of clarification: Poland here is not the country, but referring to Gregory Poland, a vaccinologist at the Mayo Clinic and Kennedy appears to be referencing this study. We’ll talk about that study in a second, but before that we need to talk about race, because what Kennedy was suggesting is profoundly racist, even if he doesn’t recognize it as such.
What is race?
Note: This discussion is not meant to be comprehensive, but rather to clarify important fundamentals for readers so that discussion of the Poland study can be performed effectively. Those who are interested in a detailed genetic examination of race are encouraged to read this chapter of the Gusev Lab’s textbook.
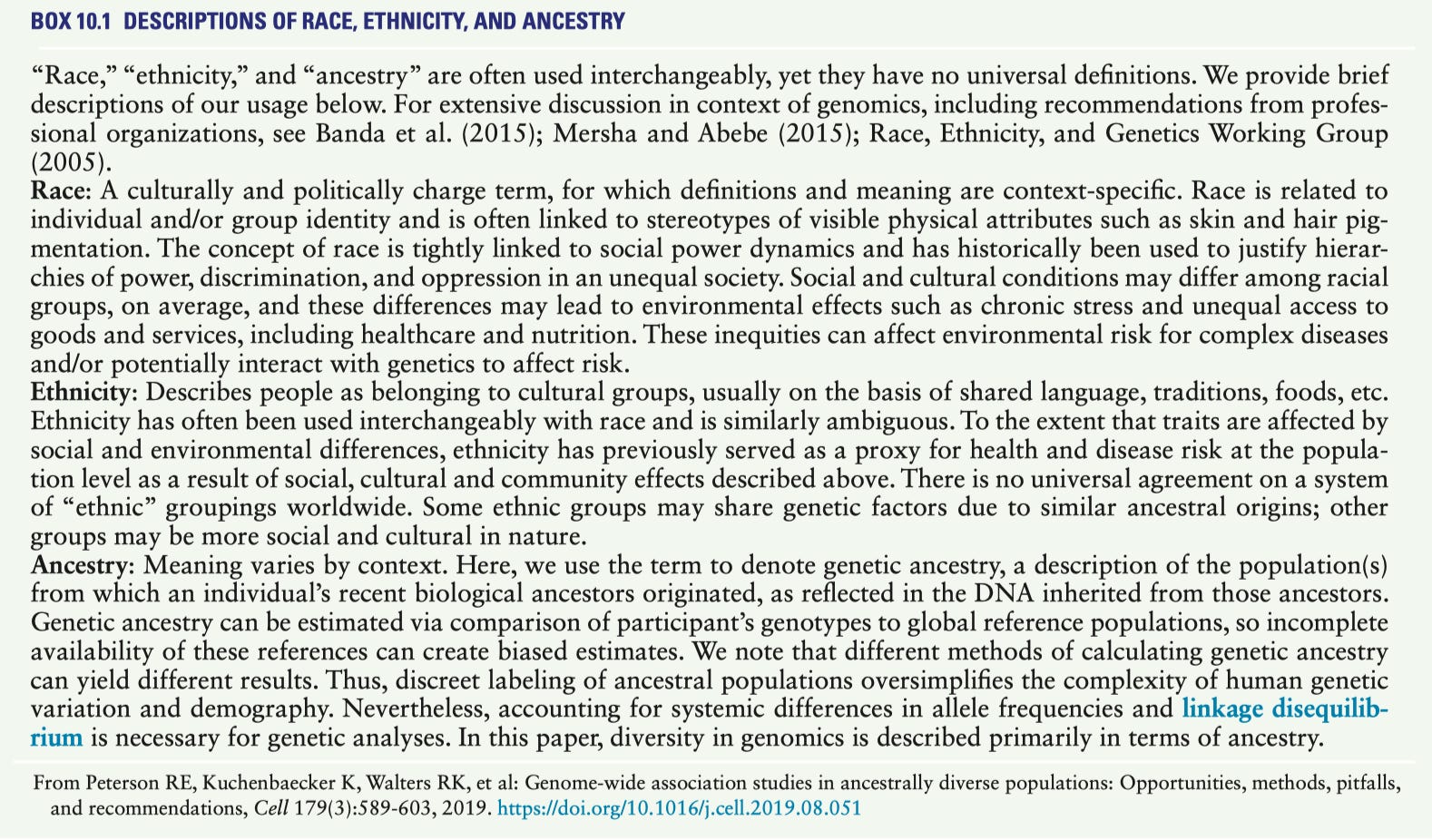
To many people, this may sound like a silly question, but a disturbingly high fraction of people who believe that get it completely wrong. Simply put, race is a social construct1. If you look across different countries, you will see that they define racial categories differently, and racial categories have also changed over time within the same country. The part where people often get confused about this point is that races often share certain physical attributes, which people erroneously interpret to mean there is a genetic basis to race, or that race reflects ancestry. The problem with this claim is that there are no clear genetic markers which can classify people into a particular race, both because racial categories are malleable, and because there is more genetic diversity WITHIN a racial group than there is between them, an insight that came from the Human Genome Project. Thus, genetics is not informative about a person’s race because race does not necessarily reflect ancestry2. As put by Jobling and colleagues in Human Evolutionary Genetics 2nd Edition:
Furthermore, genetic information, in fact, refutes any scientific basis for racism as the existence of discrete human groups. It can therefore be used to argue that racism—the belief that discrimination between apparent groups is justifiable—is an entirely social construct.3
Race is also frequently confused with ethnicity, but these are not synonyms. Ethnicity includes common ancestry, shared beliefs, cultural traditions, religion and language in addition to race.
Often when people hear that race is a social construct that does not accurately reflect underlying biology, they assume that racial categories have no meaning, but this is also incorrect. The race into which someone is grouped has profound consequences for their health within a given society, and is considered one of the most important social determinants of health4, though, more properly, the social determinant of health here is racism5. Racial categories often exist along some hierarchy which privileges some groups while penalizing others, thereby reflecting differences in exposures and risk factors, thus enabling racism to influence health in profound ways. This also means that many epidemiological studies ask about race as a variable even when it is not the subject of the study because it can be a source of confounding (although the way in which this has been done has been criticized by some epidemiologists).
A note on Founder and Bottleneck Effects
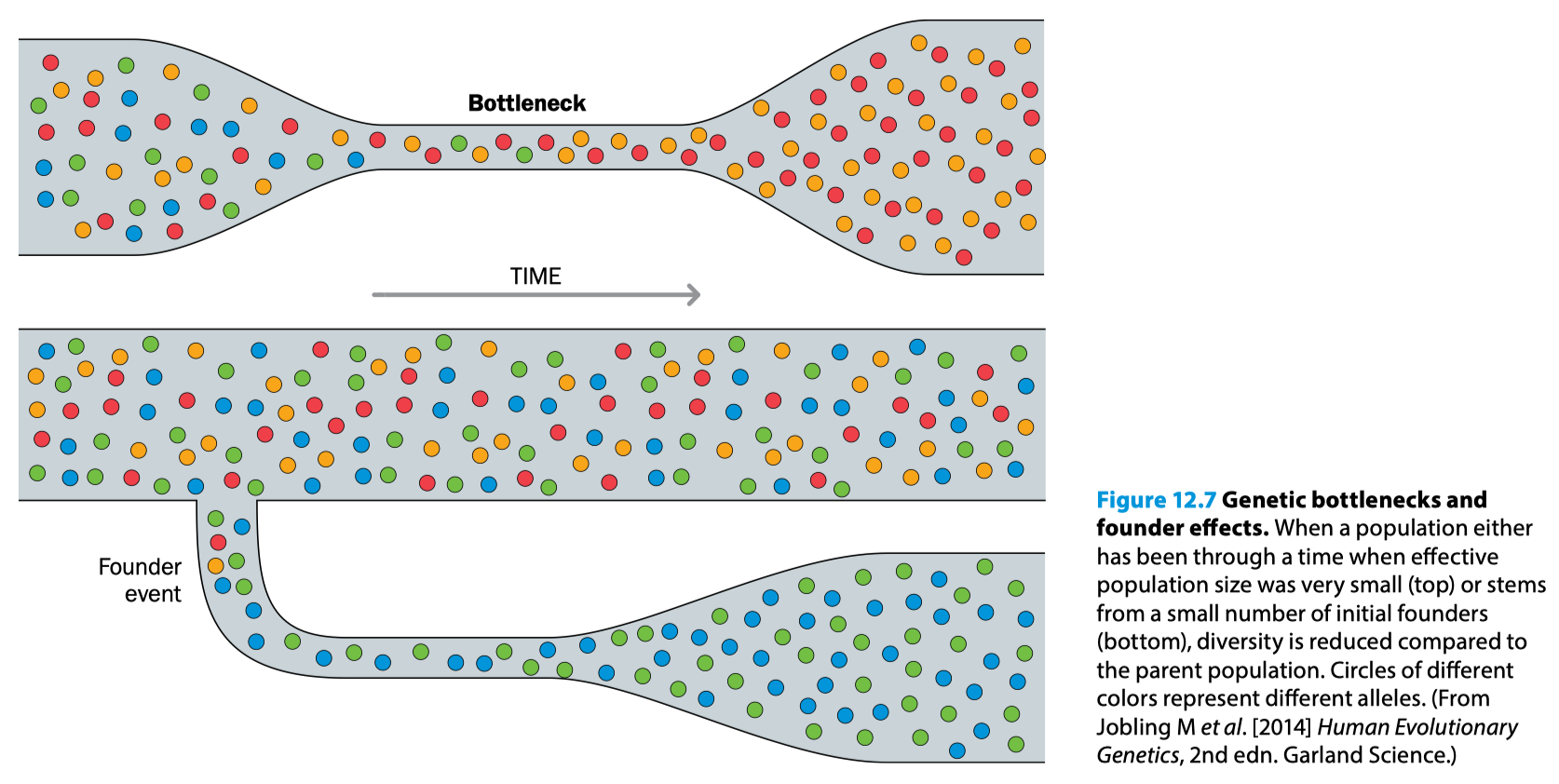
Within evolutionary biology and population genetics there are phenomena known as founder effects and bottleneck effects. Both of these reflect a situation where genetic drift (the “random” change in allele frequencies in a population over time) is drastically accelerated. The basic idea is that if a subset of the population becomes isolated from the rest of the population (e.g., if the rest of the population dies from something the subset does not, which is known as a bottleneck, or from geographic isolation which produces a new founder population), that subset of the population then reproduces within itself. This eventually results in a new population with genetic characteristics far more similar to the founders/bottleneck survivors than to the population from which the founders derived.
The significance of this is concisely explained in Human Molecular Genetics 2nd Edition by Strachan and Read (emphasis mine):
Anthropological races were assumed to have separate ancient origins and to be associated with specific biological, behavioral, and cultural differences. If these assumptions were supported by genetic data, then “racial” affiliation should predict individuals’ genotypes. Although genetic information, when harvested from a large enough number of genetic loci, can be used to predict quite accurately an individual’s birthplace (Figure 14.9), the reverse —predicting genotype from birthplace—is not possible. This is because alleles that have a frequency of more than a few percent in any given population tend to be shared by many populations across the world (see Figure 14.8B). On the other hand, those genetic markers that are confined to specific continental regions tend to have very low frequencies, which means that although there are many of them, each individual has a low probability of carrying any particular one. This, in turn, means that typically no single genetic variant, whether associated with a particular phenotype or not, contains much information about individual ancestry.
A corollary of this within humans is that certain genetic traits are more enriched within particular racial and ethnic groups- but the existence of a given genotype or phenotype cannot be inferred from someone’s race. Occasionally, we see that certain genetic conditions are much more common in some racial or ethnic groups than others; this can make certain populations particularly useful for studying particular genetic diseases:
It is worth mentioning that infectious diseases are a VERY strong selection pressure for particular phenotypes (and by extension genotypes). Cystic fibrosis seems to have evolved as a defense to infectious diseases, but the specific one is contested; candidates include typhoid, tuberculosis, and cholera). ApoL1 seems to have evolved as a defense against trypanosomiasis. There is broad consensus that CCR5∆32 (a gene required for entry of R5-tropic HIV viruses into cells, which cannot be used in the case of this variant) arose in response to an infectious disease threat but there is disagreement over what specific threat it was (major candidates are bubonic plague and smallpox), and malaria is responsible for an incredible number of human genetic changes.
Knowledge of which types of conditions are more likely in particular racial or ethnic groups can help to ensure a more timely diagnosis and treatment or inform screening decisions. This does not mean that race reflect ancestry, but rather, that certain ancestry is more likely to be found in a particular race. However, there is also a substantial contribution to the disproportionate risk of some races for certain health problems as a result of exposure to racism.
There are also significant misperceptions in medicine about how race relates to health and this has had profound consequences. For example, seemingly based on an underlying assumption that black people have more muscle mass and therefore would be expected to have higher levels of creatinine in the blood, when kidney function was estimated, the threshold for kidney disease had to be higher for black people to count as dysfunction (the equations for estimating kidney function incorporated a coefficient for race). Though the difference was small, it has major consequences because priority for a kidney transplant depends on the stage of kidney disease, and by elevating the threshold, black people with the same extent of kidney disease would be less likely to receive transplants. The NHANES survey from 2015-2018 found that:
Without the MDRD eGFR race adjustment, 3.3 million (10.4%) more Black Americans would reach a diagnostic threshold for Stage 3 Chronic Kidney Disease, 300,000 (0.7%) more would qualify for beneficial nephrologist referral, and 31,000 (0.1%) more would become eligible for transplant evaluation and waitlist inclusion.
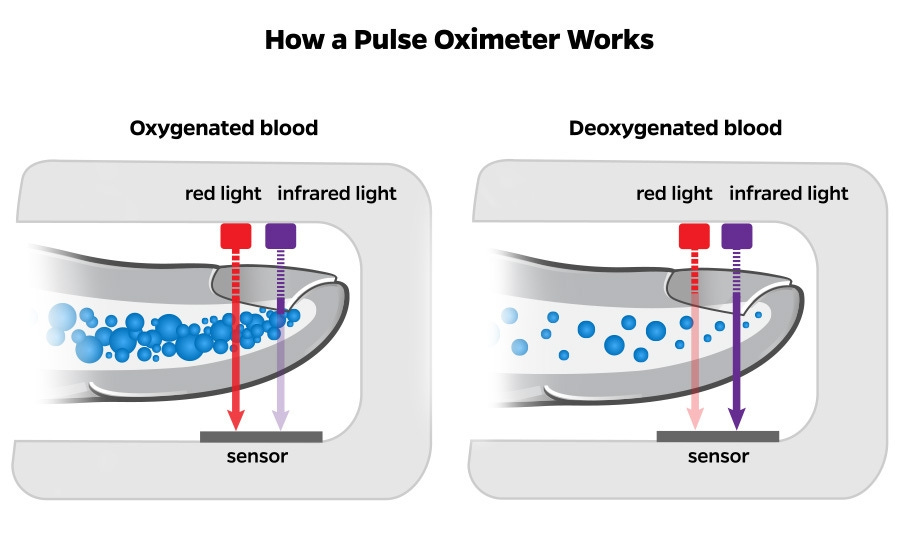
Another example has to do with pulse oximeters: these devices measure the blood oxygenation level by examining the difference in the wavelength of hemoglobin with oxygen bound and hemoglobin without oxygen bound. However, these devices were originally tested on people with paler skin, and it turns out that on darker skin, they commonly overestimate the degree of oxygen saturation, which can mean black people have delayed treatment or are not recognized as having low oxygen levels.
Another issue is reference ranges. In essence everything in medicine is based on how the values of the thing you are measuring fall along a distribution of values from a reference population, and you then declare thresholds for what is normal based on the values that are likely to associate with a disease (or not). The issue, however, is that thresholds for normal are often based on reference groups that greatly overrepresent (relative to their proportion in the population) white male adults, and so there can be instances where those metrics are inappropriate, or adjustments are made inappropriately. For example, recognizing that sexism is distinct from racism, the normal range for hemoglobin is commonly set to be lower for women because of their menstrual cycle6. However, there is no actual evidence to suggest that this adjustment to the range is warranted, and furthermore, the incidence of iron deficiency among women in particular is staggering (note that anemia is a late sign of iron deficiency). Another example has to do with the levels of neutrophils (the most abundant white blood cell in the body). A condition unfortunately named benign ethnic neutropenia (BEN) refers to a state in which people have lower than normal levels of neutrophils but without evidence of an immunological problem that could arise from inadequate neutrophil function. This condition is far more common among those with ancestry from the sub-Saharan part of Africa than in those of European descent because the genetic driver also confers resistance to malaria. Lack of knowledge among clinicians of this condition can result in unnecessary invasive testing to determine the basis for the low neutrophil counts, including bone marrow biopsy.
One last point: many people would dismiss these disparities on the basis of the idea that racism has to be explicit between individuals with malicious intent. The fundamental reality is that if we want a society where people genuinely have an equal opportunity to succeed, the intent is much less important than the effect. Race should not be a factor in determining health outcomes, and yet, it is. The point of finding these disparities and addressing them is not about a witch hunt to blame an individual for creating policies that disadvantage people of a particular race, but rather to acknowledge that the systems in which we exist perpetuate these disparities and work to make life and health better for everyone. Why should we have pulse oximeters that work more poorly for people of a particular race? Or adjust measures of kidney function in a way that results in fewer people of a particular race getting appropriate care from a specialist? There is no good reason unless you believe in a natural hierarchy between the races- and there’s a word for that.
The Poland Study
First, it should be noted that Kennedy is not raising this canard for the first time in the Senate hearings, but rather, building upon a legacy of exploiting the abuse of minoritized groups to sow further distrust in vaccines, an intervention that is particularly important in light of the racial disparities in vaccine uptake in the US. Gregory Poland, the corresponding author of the study, has previously addressed the problems with Kennedy’s approach. In brief, he noted that:
The sample size was too small for reliable conclusions to be drawn about the vaccination of entire racial groups.
Another interpretation of the findings is that rather than black and Somali people getting too much vaccine, other racial groups are getting too little.
No evidence, including from the study, supports the idea that black people are being overdosed with the rubella vaccine (or any other vaccines).
The differences in the immune responses do not consider immune history- it is possible that study participants from Somalia were more likely to be previously exposed to rubella in refugee camps before coming to the US, and so the vaccine was functioning as an additional exposure, which those from the other racial groups avoided.
All of these points are valid, but I would like to extend these a little bit. In what is probably the most comprehensive review of factors influencing the immune response to vaccines, Zimmerman and Curtis gave us this very nice figure:
You will notice that race is nowhere on here. Race can be tightly associated with some of these factors, such as the nutritional factors (which often reflect, at least in part, socioeconomic status), the environmental factors (some communities are enriched with particular racial groups- again, socioeconomic status), etc. which can give the illusion of an effect of race, but, race is a bystander here. There are other biological explanations for the differences in the immune responses based on these factors, but race may be correlated with them (remember that- it’ll become important later). Today, to understand what specific biological factors influence the immune response to vaccines (in pursuit of improving the immune response), we have an approach known as systems vaccinology: we can simultaneously measure may different factors (like which genes are expressed throughout the course of an immune response, which metabolites are more or less abundant, which pathways are activated vs. inactivated) and associate these with the quality of the response to the vaccine. Then, once we see which factors associate with better or poorer responses, we can validate them experimentally by manipulating them in cell culture or in preclinical models (usually mice) to see whether we are looking at a bystander or a real effect. For example, system vaccinology was used recently to identify that megakaryocytes (the cells that make platelets) promote the survival of plasma cells (which make antibodies) leading to more sustained antibody responses, and vaccines that induce a stronger megakaryocyte response have more durable antibody production. Once systems vaccinology identified the association, a cell culture model demonstrated that the effect was real and mediated both by physical contact between the plasma cells and the megakaryocytes and production of plasma cell survival factors. Then a hormone that promotes megakaryocyte development (thrombopoietin) was used to compare the antibody response durability in mice, and it worked- mice that received a vaccine with thrombopoietin had consistently had higher antibody levels at all measured timepoints at 63 days post-vaccination. Through this approach, we now have a marker we can look at for the study of new vaccines to help gauge the likely durability of an antibody response and we have a lead for a potential mechanism to enhance the durability of the immune response to future vaccines.
The study led by Poland seems to have attempted to approximate something similar here, but it makes a cardinal sin in that it tries to use genetics to classify people’s race:
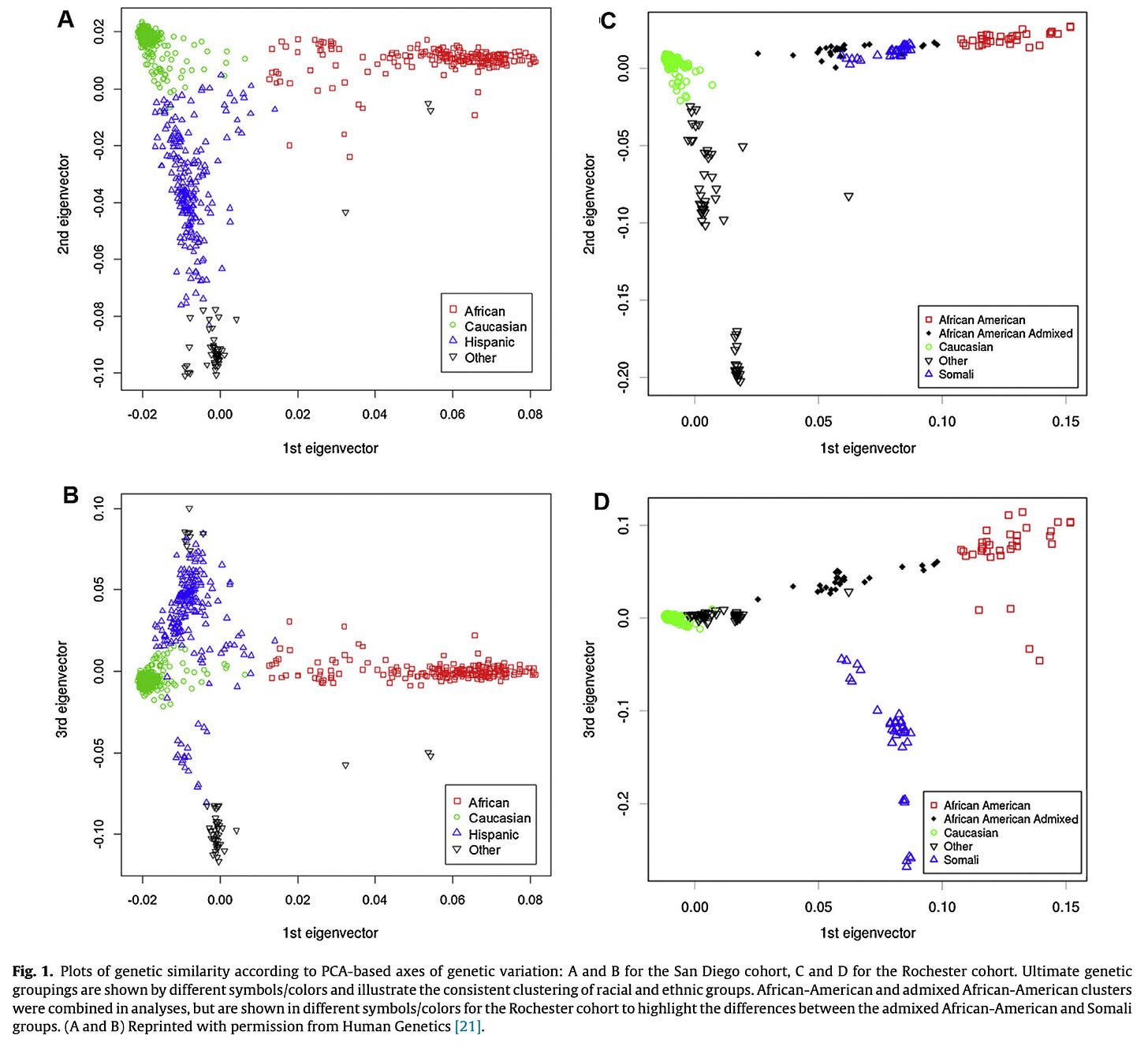
This is unhelpful because it does not give us any insight into the actual biological mechanisms that might be driving the differences, which would be the goal here because the nature of the study is immunological, not epidemiological, and because you cannot use genetics to assign race. Genetics can be helpful in determining ancestry because of the founder and bottleneck effects, but race does not inherently reflect ancestry. Nonetheless, let’s pardon this for a moment and consider the actual responses observed by “races” here:
In both cohorts, the neutralizing antibodies are higher in the Somali and the African American cohorts respectively- but every other parameter of the immune response is not meaningfully different. There is also a second question raised here: does the difference in the level of antibodies identified here actually translate to a meaningful difference in protection? Here is a summary from Plotkin’s Vaccines 8th Edition concerning what we know about biomarkers for protection against rubella (correlates of protection):
The immune response that correlates best with protection is neutralizing antibodies. 451 Nonetheless, even vaccinees with low levels of serum antibodies are often protected, 452 while reinfection may take place in some individuals with measurable antibodies. Because measurement of neutralizing antibodies is not routinely available, 15 IU of antibodies measured by other methods has been proposed as a correlate of protection. 453 However, infants with CRS have been born to mothers who have antibody levels of 15 IU/mL or greater. Review of epidemiologic data in the United States demonstrated protection at 10 IU/mL, so the cutoff for protection was set at 10 IU/mL in the United States. 152 Although there is some variation among countries in terms of the concentration of IgG antibodies considered to be protective, the presence of rubella IgG antibodies greater than or equal to 10 IU/mL is commonly considered to provide evidence of protection (WHO immunological basis for immunization).160
Although cellular immunity seems to have little correlation with protection from replication, arrest of viral excretion by CRS patients correlates with the appearance of specific lymphoproliferation responses.454
A complicating factor in the interpretation here is that we are given a neutralizing antibody titer reported as an NT50 value, which is much more involved to measure and cannot be done at scale practically and cannot be converted to the binding antibody titers described as being measure of protection. Nonetheless, one of the first comments made in this passage is that even people with very low serum antibodies may be well protected against rubella. In other words, while it is likely that those with higher levels of antibody would be able to be exposed to a bigger dose (inoculum) of rubella virus, we do not know whether it is likely that any of these study participants would encounter the relevant doses in the real world as a means of exposure to rubella, meaning we cannot infer that there would be a tangible difference in the level of protection here. In particular, rubella has a long incubation period and replicates relatively slowly- a major factor that likely underlies the finding that those with low antibodies can still be well-protected is the ability to mount a rapid recall response using their memory cells to stop the disease. No metrics here are offered concerning the memory cells of the study participants, so no conclusions can be drawn directly about the protection elicited. Furthermore, it is worth taking note of the fact that though the antibody titers may differ between the groups the other parameters of the immune response measured do not significantly differ.
Another major issue with taking this study as evidence of the entire vaccination schedule requirements needing to be lower for black people with regard to the exposure to antigens is that a more robust response to rubella (again, with all the caveats therein) does not automatically translate to more robust responses in general. A critical determinant of the quality of an antibody response is the ability of the B cells to get help from T cells. This in turn depends on the ability of the B cells to effectively present antigen to the T cells, which depends on the binding avidity of the antigen-presenting machinery (MHC class 2 proteins- in humans these are also known as HLA-DR/DQ/DP) to the peptides of the antigen:
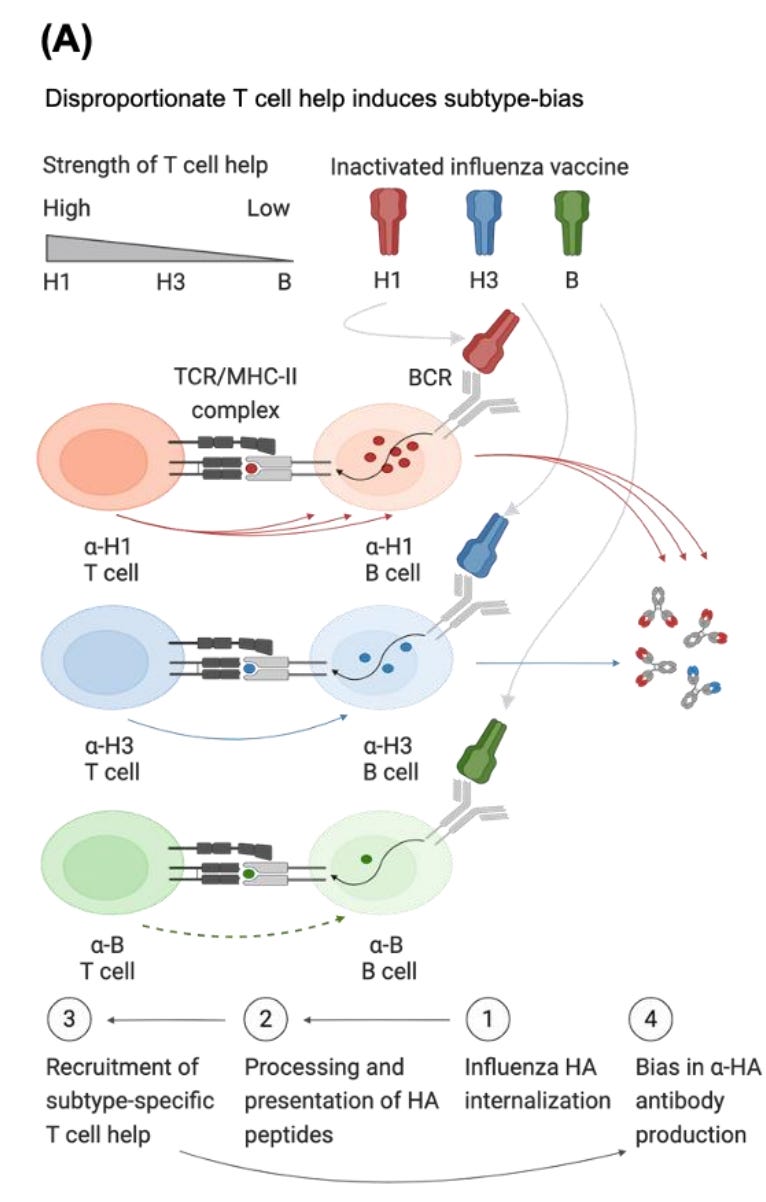
Recent work has shown that this is likely a dominant factor in the bias people have to particular influenza subtypes, stronger even than the effect of their immune history (which in turn points to a workaround but that can be the subject of a different post). However, the MHC alleles that are most beneficial for a particular antigen are specific to the antigen and they are genetically determined. For example, one study found that hepatitis B vaccine responders were more likely to have DRB1*01 (DR1) and DRB1*15 (DR15) alleles and non-responders were more likely to have DRB1*03 (DR3) and DRB1*14 (DR14). For SARS-CoV-2, HLA-DQB1*06 was associated with higher levels of antibodies against the spike protein receptor binding domain. The idea that you can use a response to a single vaccine antigen to make global conclusions about how all vaccines on the schedule should be administered demonstrates a profound lack of awareness of some of the most important fundamentals of immunology. An important detail in this point: the MHC locus on chromosome 6 is a haplotype- it is essentially always inherited together, and therefore tends to be strongly associated with ancestry. Again though, at most this is all speculative because this study did not gather that data. There are other potential biological reasons that could explain these results, but I hesitate to offer them because they require too many assumptions without any actual evidence.
ETA: Epidemiologist René Najera also had these insightful comments:
I do want to clarify one point: Kennedy’s claim is not racist simply because it attempts to suggest different vaccination requirements for people on the basis of race/ethnicity. There are instances where that is relevant. For example, the Haemophilus influenzae type b (Hib) vaccine given to Alaskan Natives and American Indian children is preferentially the PRP-OMP version of the vaccine, which elicits a superior response, because these demographics have a disproportionately high risk of invasive Hib disease. Note the difference here though: there is a specific condition for which there is a disproportionate burden and a sound scientific rationale for this choice and it is not based on imagined biological characteristic of children from these racial/ethnic backgrounds but a true epidemiological finding of greater risk. Kennedy wants to privilege a small study lacking in critical data because it confirms his biases that “vaccines are bad” and he sees a profit motive- just as he does with every other issue relating to vaccines, especially the falsity that vaccines contribute to autism, a question for which there is possibly more scientific evidence than any other single question in science including well-designed studies of millions of children across multiple countries.
In sum, the idea that black people need a different vaccine schedule is a continuation of a long history of systemic racism and stands to pose major harms to both the black community, and everyone else because it would contribute (certainly in the form Kennedy is proposing) to the erosion of herd immunity.
As a brief primer for some of the relevant vocabulary here:
Genotype: The specific sequence in the genome that may result in a particular observable trait.
Phenotype: The observable trait that is expressed e.g., hair color, eye color, skin type, presence/absence of a disease.
Allele: A variant of a gene.
Mutation: A change in the sequence of a gene relative to some reference allele.
Dominant: A single copy of the allele is enough to produce the trait.
Recessive: Both copies of the allele are necessary for the trait to be expressed.
Homozygote: Individuals who have the same copies of an allele; adjective- homozygous
Heterozygote: Individuals with two different alleles for a particular gene; adjective- heterozygous; occasionally the term compound heterozygote may be used, referring to a heterozygote which has two recessive alleles.
Hemizygous: The state of having only a single copy of a gene. For example, the sex-specific region of the Y chromosome in people with a single Y chromosome or the X chromosome in people with a single X chromosome.
Co-Dominant: Both alleles are expressed simultaneously, producing the phenotype of both simultaneously. For example, if a person has the allele for A type blood on one chromosome, and B on the other, they will have type AB blood which has both the A and B antigens on the red blood cell surface.
Incomplete dominance: Both alleles are simultaneously expressed but the phenotype is an intermediate between the homozygous
Mendelian: Following simple rules of dominance and recessiveness; influence from other genes is negligible. Most traits do not follow Mendelian inheritance and many traits commonly described as having Mendelian inheritance do not e.g., eye color.
Epistasis: The state of a gene’s expression being influenced by another gene.
Autosomal: Inherited through non-sex chromosomes (i.e., everything not encoded by the X or Y chromosome).
Sex-linked: Inherited on the sex chromosomes, which almost always means X-linked because the Y-chromosome has minimal genetic information. This means that people with XY chromosomes will always express the trait (even if it is recessive); those with XX chromosomes may need both copies of X to have the genotype in question, if it is a recessive X-linked trait.
Haplotype: A group of genes that are inherited together from a single parent (because exchange between the maternal and paternal chromosome copies does not occur over that region when gametes are being made). For example, the MHC locus on chromosome 6 (in humans) is essentially always inherited in the form it appears on a single chromosome, so it is known as an MHC haplotype.
People trying to engage in scientific racism (even if they vehemently deny that’s what they’re doing) have been known to invoke a few additional points that I feel merit addressing preemptively.
The first is the notion that race is actually well exemplified within genetic theory as a biological concept but because it is not “sociopolitically palatable” to call it such, the term “population structure” are used instead. This argument demonstrates a profound ignorance of genetics because these terms are not synonymous. Population structure is the set of factors that influence the likelihood of two gametes coming together in a fertilization event. Examples of these factors include the system of mating, the amount of genetic interconnection with other demes, the randomness associated with the size of the deme, and the age structure of the deme (a local geographic population of reproducing individuals that has physical continuity over time and space and in which most of the acts of reproduction occur between individuals who are members of the same deme). There is a broad consensus among geneticists that you cannot define human races through genetics.
Another point people make is an attempt to draw an equivalence between that concept of race and subspecies. To start with, the concept of a species is extremely fraught with a number of different definitions depending on the context, which makes the idea of a subspecies at least as fraught. Nonetheless, a metric called the fixation index (or FST where “S” stands for subpopulation and “T” stands for total population) which reflects the extent to which subpopulations are genetically similar or different. If the fixation index is 0, it means that at the examined regions of the genome, the subpopulation is identical. A value of 1 means that at the examined regions of the genome, the subpopulations differ at every point. Some sources (particularly older ones) argue that a value of 0.25 or higher is enough to distinguish subspecies and therefore races, so, if such a value occurs between two subpopulations, they can be considered different races. In general, no one within the field of genetics thinks about races in this way because the cutoff of 0.25 is completely arbitrary, the fixation index is sensitive to what particular regions of the genome you examine (choose something highly variable like microsatellites and it may go up), and even when this metric is used for large groups of subpopulations, you don’t attain 0.25. Now, some people can cherry-pick references to argue that two subpopulations have a high enough fixation index that this threshold is met, but the fundamental reality is that this metric is extremely malleable. It’s worth mentioning that classic hereditarians expected the fixation index to be very close to 1 between racial groups, which does not occur in any actual dataset.
Social determinants of health refers to non-medical (i.e., non-biological) factors that influence health outcomes.
Ordinarily, I would use more inclusive language here (i.e., menstruating persons) but iron deficiency in transmen is less of an issue because of testosterone enhancing iron absorption, and for other forms of gender diversity, I am not aware of any data specifically examining their risk of iron deficiency.