A Vaccine Did Not Cause the Mother of All Pandemics
RFK Jr. recently claimed on Joe Rogan's podcast that there is good evidence that the 1918 influenza pandemic was vaccine-induced. This is complete nonsense- but the real history is worth knowing.

It’s been a while since I last published anything here (I have multiple long-form posts that are in various stages of completion and am working on getting them through in the most expedient manner I can muster). I interrupt this hiatus (is it a hiatus if you have been working on the thing during the gap?) largely for the fun of looking at some truly interesting scientific history and to take you through the anatomy of a really important scientific discovery: how we know what caused the 1918 influenza pandemic (if you said “influenza,” you get a gold star- although that’s a bit of a gimme). But first, let me tell you a bit about why I’m writing this (you can skip this part if you just want to know the history).
You may be aware that Robert F. Kennedy Jr. was recently featured on Joe Rogan’s podcast where Rogan credulously allowed him to spew antiscience and in particular anti-vaccine propaganda for about 3 hours. Kennedy and his organization are among the most prolific sources of vaccine canards that exist. I truly don’t know how many people have died or suffered because they entertained anything he has to say on the matter (but I’d go out on a limb and say it’s not less than 83). Anna Merlan at Vice wrote a really nice article calling out Spotify for their irresponsibility in continuing to support Rogan’s podcast despite his dissemination of scientific and medical disinformation that could literally get people killed1. This resulted in a deluge of harassment against internationally renowned pediatric infectious disease physician-scientist, Dr. Peter Hotez, after he refused to come on Rogan’s podcast to debate vaccines with Kennedy, and as I (alongside the amazing Professor Gavin Yamey), as well as others have explained he was absolutely right to do so. Anyway, in a demonstration of truly herculean, supererogatory patience, my pal Dr. Daniel Wilson sat through this festival of firehosing and addressed the seemingly endless mendacities that emerged (I have chosen a specific timestamp):
When I remarked on the sheer absurdity of this proposition (it seemingly requires one to believe that vaccines could travel backwards into time and vaccinate people- which, in fairness, is a real thing that Naomi Wolf has claimed so it is very hard to know what the provenance of these claims often is) that the 1918 influenza pandemic was a “vaccine-induced flu” on Twitter, Kennedy acolytes came out of the woodwork to defend the claim. It turns out there is more nuance to this claim than I initially realized, but unfortunately for Kennedy, there isn’t more accuracy.
I’m not writing this for the benefit of anyone who thinks that Kennedy is right on this issue or broadly because that perspective requires not so much logical leaps as much as logical levitation. It would take literally thousands of pages to rigorously address the nigh-innumerable false or misleading claims Kennedy has made about vaccines over the years (I do have a day job- although Skeptical Raptor, Orac, Vaxopedia, and Science-Based Medicine have been absolutely punctilious about addressing them, so I would encourage anyone interested in specific claims he made to search there first). These individuals don’t believe Kennedy because they think he made some truly compelling, cogent arguments, because (whether they realize it or not) that is not enough- to believe Kennedy on vaccines would require acceptance of an extensive conspiracy on the part of multiple industries, corporations, governments, professional medical expert bodies, public health professionals, physicians, scientists, nurses, etc. that is quite literally so unlikely from a purely probabilistic perspective that it may as well be impossible and that is BEFORE you start considering the substance of his claims. The people who believe Kennedy do so principally because they believe he (or his organizations or his acolytes) is more trustworthy than the aforementioned professionals (and while there is a critical and lengthy discussion to be had about the reasons for that, I am not going to do it on this specific post). This choice is an emotional one- it does not occur on the level of reason and so I cannot reason them out of it (not without some fairly extensive buy-in of trust currency in me at least requiring a very substantial investment of time that I, unfortunately, do not have at my disposal at the moment). However, what I can do and what I want to do here is to show to those who are genuinely interested how we learned about the cause of pandemic influenza and how we know it wasn’t a vaccine.
The History of Influenza Virology
For a detailed account on the 1918 pandemic itself, you can’t do better than The Great Influenza. The CDC also has a very informative summary.
The question of whether influenza is actually influenza is a fairly interesting diagnostic challenge if you think about it (and subtract a modern understanding and methods of microbiology, virology, etc.). Indeed, in the pre-microbiological era (which here I will take to be pre-1876 as this is when Robert Koch published his seminal work on anthrax), it was not all that easy to distinguish influenza from the many other microbes that made life too short and difficult. Similarly, it wasn’t clear whether influenza-like illnesses between influenza pandemics were influenza or something else (again- no way to distinguish between influenza viruses and, say, coronaviruses because neither the technology nor the understanding of infectious diseases existed to differentiate them) and vital statistics were not around until about the mid-1800s (the British disease registry was first set up in 1836). Nonetheless, we do know that the 1918 pandemic, what has been called “The Mother of All Pandemics” “The Great Influenza,” and “Spanish Flu” was caused by an H1N1 swine influenza- and this fact alone makes it impossible for it to have been caused by a vaccine.
Before this Great Influenza however, there were at least 4 major smaller influenza pandemics which incrementally contributed to our knowledge of the disease. By the 1890s, two major works had concluded that influenza was a distinct, communicable disease that spread more rapidly than any other communicable disease but not faster than human travel. Health officials of the time realized that mild influenza was basically impossible to distinguish from any number of other respiratory illness but concluded that the pandemics of 1889 and 1848 were also both caused by influenza. The 1889 pandemic suggested that pandemic influenza had huge morbidity but a relatively low mortality rate which had an age-specific pattern: 20 to 40 year-olds were the most likely to contract it while those over 50 were the least likely, and the older one was, the more likely the case was to be fatal. Still, the cause of influenza was not known.
In 18922, Richard Pfeiffer reported that he had found the cause of influenza: Bacillus influenzae, which today is known as Haemophilus influenzae3. Pfeiffer stated that the microbe had been isolated from every case of influenza he examined- which makes some sense because this bacteria is present in the upper respiratory tract of most healthy adults as part of the microbiota (of course, this was not known initially). Pfeiffer’s bacillus was very persnickety about culture conditions (refusing to grow on anything other than blood agar4) and proved difficult to classify by the microbiological methods Pfeiffer had used5. Furthermore, Pfeiffer could not satisfy Koch’s postulates to show that this bacillus caused disease despite multiple attempts with many animal models (even monkeys). Nonetheless, when the bacterium continued to be isolated from influenza patients (although not by all investigators6), coupled with Pfeiffer’s authority as a direct disciple of Robert Koch, this claim was more or less accepted- a compelling alternative explanation did not yet exist, and samples were relatively limited because the 1889 pandemic had resolved. However, in 1906, the first challenges to this hypothesis emerged when in a series of 18 patients with influenza, just 3 of them were found to have the bacillus. Could it be that this wasn’t the cause of influenza after all?
The 1918 pandemic gave a chance to study this question through the new and exciting field of virology7. Berkefield and Chamberlain filters in essence made the field of virology possible through the concept of filterable agents: the filter was so fine that B. influenzae (or other bacteria) could not pass through it because it was too large (at least this was the theory- in practice in the early 20th century the production of these filters was not yet mastered and they proved variable in their ability to exclude bacteria). If the patient’s secretions were filtered and disease occurred on infection, it meant that the responsible agent had to be either a virus or a toxin (or potentially mycobacteria which were smaller than typical bacteria). First, in September 1918, French researchers Nicolle and Lebailly reported filtering the secretions and infecting two healthy volunteers, an early clue that bacteria were not responsible. Still, this small study could hardly be definitive and other investigators had difficulty replicating it. In 1919, Yamanouchi and colleagues conducted a larger experiment in a Japanese cohort with 24 volunteers and found something significant: 6 of them, who had previously had and recovered from influenza, did not become sick (but the remaining 18 did). Influenza had not been removed by filtering. In another set of experiments, 14 healthy individuals who had not had influenza (how this was confirmed is not clear) were given either Pfeiffer’s bacillus or a cocktail of microbes isolated from influenza patients, including Pfeiffer’s bacillus- none developed disease. They summarized their results:

Still, this didn’t automatically prove virus. It could be that the patient specimens contained a toxin that caused influenza- and that toxin could have come from a bacterium.
Then, in 1920: Olitsky and Gates took secretions from patients actively ill with influenza from all 3 waves of the 1918 pandemic and between them, and they filtered the secretions through a Berkefeld filter. When Olitsky and Gates used these secretions to inoculate rabbits in their lungs, the rabbits rapidly developed a disease resembling influenza, even though the bacillus had been excluded. The idea that it was a toxin was disproved in Olitsky and Gates’s same study when the lungs of infected rabbits showed the ability to cause many successive infections in other rabbits, indicating that the cause was replicating (a toxin would have lost potency as it was diluted from host-to-host and eventually failed to cause disease in new hosts): influenza had to be caused by a virus.
Despite this, people hesitated to accept that Pfeiffer was wrong. Clinicians did not want to believe in something they themselves could not see (and the electron microscopy required to see most viruses had not yet been invented). 1918 influenza eventually faded back into a seasonal pattern and did not cause pandemic-level morbidity and mortality, and so interest in the disease and access to clinical samples died down. However, the 1918 pandemic influenza virus also gave rise to what was called “hog flu.” The virus jumped from humans into pigs and caused influenza in the fall of 1918 where it then split into 2 lineages (a human and a pig one). In 1931, Shope published a series of papers which demonstrated that indeed this swine influenza was the same influenza that defined the 1918 pandemic (Shope is generally credited with being the one who deduced that influenza was caused by a virus). This was important because it also reignited research interest in influenza.
Some of the seminal work therein came from Smith and colleagues in 1933 (this is generally the work that is credited with isolation of influenza virus). In 1933, there had been another influenza epidemic, which offered the opportunity to study the question again. Secretions from influenza patients were again filtered and cultured to prove there were no bacteria, and these were inoculated into ferrets (ferrets have seen much use as models for influenza especially, as well as and other respiratory viruses). First, they found that ferrets were immune to the same strain of influenza after they recovered from it (but Smith and colleagues astutely noted that it was not clear whether they would be immune to other strains- but they were protected from swine influenza supplied by Shope which they took to mean that the two viruses were very similar antigenically). They also traced protection to neutralizing antibodies in the ferret’s serum that was present after recovery but not before, and demonstrated that humans who did not have influenza also lacked neutralizing antibodies. At the same time, human sera did not always work to protect the ferrets, even when neutralizing antibodies were present. In the same year, Dochez and colleagues developed a method to culture influenza in embryonated chicken eggs, and a few weeks later, Smith and colleagues showed that the virus could be serially propagated in ferrets. We now had the most important tools needed to study the virology of influenza. In 1936, Shope furthermore showed that those who had antibodies to influenza were able to neutralize the swine influenza virus, supporting once more that the swine flu and the 1918 pandemic were closely related. In 1936, Thomas Francis Jr. also discovered influenza B viruses.
Still, we know quite a bit more about the cause of the 1918 pandemic than just that it was influenza- we in fact have been able to reconstruct its genome and have studied it in animals to see why it was able to cause such devastating disease (it’s honestly still not entirely clear). The challenge, however, is that influenza is an RNA virus. Its genome is extremely fragile (on the chemical level), and as time went on, it would be increasingly unlikely to be able to find authentic virus isolates, let alone reconstruct the genome. But, there was an answer: permafrost graves. Expeditions in 1951 by Hultin, McKee, and Layton to Brevig (where 90% of the population had died in the 1918 pandemic) where they exhumed the bodies of those who died in 1918 and took extensive samples from their lungs and stored them in sterile conditions and dry ice. These cold conditions could protect the RNA genome of influenza, making it possible that we might learn more about that virus. The team returned to the lab and proceeded to inoculate their ferrets with this tissue samples they hoped would contain this historic virus- but the ferrets did not become sick. Cultures from the lungs grew Haemophilus influenzae (Pfeiffer’s bacillus) and Streptococcus pneumoniae, which was evident on lung histopathology, but viral pneumonia could also be seen on histopathology. Still, this “time capsule” did not contain replication-competent influenza virus as far as they could tell.
This work went untouched until 1995, when Jeffrey Taubenberger at the NIH undertook a project to recover the RNA fragments of the 1918 influenza virus. While those permafrost-preserved bodies did not have the answers, there were other time capsules. Tissue samples had been preserved in formalin from the 1918 pandemic at the National Tissue Repository of the Armed Forces Institute of Pathology (AFIP). Combing through the autopsy reports of a number of those who died in 1918, 100 of those who died from influenza were identified. Of these, 70 had tissue samples, and of those just 13 had a reasonable chance to contain pieces of influenza’s genome- and one of them did. These tiny fragments showed that the virus was an H1N1 influenza related to the currently circulating viruses that infected humans and swine, rather than bird as was initially believed8.



While this was a major breakthrough, this does fall quite a bit short of an influenza genome. As fate would have it, Hultin (the very same one from the 1951 expedition) read Taubenberger’s paper- and offered to conduct a second expedition to Alaska to obtain more samples now that technology had advanced to a point where we could literally sequence this virus. These samples were paired with more that had been recovered from the tissue repository and showed minimal variation across the isolates. In pieces, the genome was assembled as more and more samples were collected. Finally, in 2005, the genome of the virus was reconstructed and showed more than a few surprises virologically (interested readers can check out the paper for themselves, as well as this one), and it was more virulent in mice compared to reference strains. Over the years however, animal challenge studies have produced some mixed results on the matter of the 1918 virus’s virulence. Indeed, the extraordinary death toll of the 1918 pandemic is probably most directly attributable to its novelty: people encountered a virus they had no prior immunity to and it was capable of efficient transmission from person-to-person (the basis for the mortality curve’s unique W-shape however is more complex than I care to get into here). It wouldn’t surprise me if a similar outcome were observed with any strain of influenza people had no prior immunity to (though that experiment is, obviously, not ethically permissible).
You might reasonably ask why we bothered to invest all of this effort into understanding a virus that killed so many people 100 years ago. For one thing, influenza viruses are still around. In fact all circulating influenza viruses that infect humans are thought to be descended from the 1918 pandemic strain (it is literally the Mother). This means that understanding what made the 1918 strain so bad can help us understand what makes currently circulating viruses such a problem too, and inform us on how we might prevent future devastation by influenza. A detailed accounting of some of what we have learned about influenza from the 1918 virus can be found here.
The History of Influenza Vaccines
As I said earlier, it took until about the 1930s before people accepted that the 1918 influenza pandemic was caused by a virus (influenza virus, then realized to be influenza A virus), although evidence supporting a viral cause was gathered during that pandemic. Nonetheless, influenza was recognized as a public health problem long before we knew anything about its biology. Inspired by the incredible success of smallpox vaccination (and diphtheria, typhoid, and rabies as of 1918), there were many attempts to vaccinate against influenza.
Obviously, there’s a fairly big problem here: until about the 1930s, it was thought that Pfeiffer’s bacillus was the cause of influenza, and so vaccines were (mainly) made targeting it, rather than influenza virus9. In October of 1918, Royal S. Copeland, then New York City’s health commissioner promised a vaccine from the laboratory of William H. Park. Park had successfully cultured Pfeiffer’s bacillus, heat-inactivated it, and shown that the resultant vaccine produced an immune response in animals. A 3-dose series was advised. Unsurprisingly, it did not work. Another attempt at around the same time came from Timothy Leary, who also made a vaccine based on Pfeiffer’s bacillus but fast-tracked it because of the crisis and completed all testing for it (if you can call it that) in 1 week with some animals and 2 human volunteers. The Red Cross then rapidly distributed the vaccine. Again, it did not work. Yet another vaccine was made by Horace Greeley- it also did not work. Some vaccines from the time didn’t contain even Pfeiffer’s bacillus: they were made by culturing bacteria isolated from influenza patients and inactivating them and administering those as a vaccine. We could continue to go down the list of vaccines people created during the 1918 pandemic because there were probably dozens but you get the point: none of them contained influenza, so none of them worked.
So, what did it take to actually get an influenza vaccine? Thomas Francis Jr. wrote a detailed account in 1953 and the CDC has a timeline here. In 1937, Thomas Francis Jr. and T.P. Magill published work showing that injection of live influenza virus resulted in the development of antibodies without causing influenza. In that same year, Stokes and colleagues showed that live influenza could be used to vaccinate children in a series of 3 intramuscular doses to achieve protection. In 1940, Jonas Salk and colleagues described a UV-inactivated influenza vaccine that also demonstrated the ability to induce antibodies. That same year, Francis discovered influenza B viruses and found they were the cause of an epidemic similar to influenza A but antigenically distinct from it in 1936. Attempts to make an inactivated vaccine were also carried out using formalin (as was done for toxoid vaccines in that era- and continues to be done as it is very effective) but the early attempts proved unsuccessful. In 1942, the US army began testing a formalin-inactivated bivalent vaccine (containing both influenza A and B) which proved to be immunogenic and safe. In 1943, an efficacy study (by way of human challenge with influenza A) vaccine was carried out on schoolchildren and it clearly worked:
Of 28 control individuals, 10 came down with clinical influenza following inhalation of a recently isolated active virus. Only 1 case, which had not responded to vaccination, occurred among the 44 vaccinated persons, 27 of which had been immunized 4 months prior to the exposure.
Efficacy against influenza B proved more difficult, however. A larger study (about 12000 people) was carried out in 1943 with a trivalent influenza vaccine (containing 2 strains of influenza A and 1 of influenza B) and a substantially lower rate of hospitalization was seen in the vaccinated group compared with the unvaccinated group (2.2% vs. 7.1%), except for one site in California, which was attributed to the emergence of a novel strain of influenza. A vaccine was eventually available to the general public in 1945. The importance of different strains in influenza began to gain recognition in 1947 when a study of about 10,000 individuals in Michigan found that the influenza vaccine used failed to show evidence of protection.
Adjuvants to enhance the immune responses (and therefore protection) of influenza vaccines were considered from fairly early on; lipid-based adjuvants however seemed to result in harsh reactogenicity. Salk and colleagues worked on a vaccine which was adjuvanted with a mineral oil emulsion of Arlacel-A (essentially, Freund’s incomplete adjuvant) but these seemed to result in delayed formation of cysts after vaccination. Today, there is an adjuvanted formulation of seasonal influenza vaccine for older adults (which does not have these risks), and influenza vaccines undergo a process to update their composition to match circulating strains for the upcoming season as closely as possible.
Could an influenza vaccine have caused the 1918 pandemic?
Some have proffered a false history in which the influenza pandemic was caused by a vaccine. As explained, this is vacuously false because the influenza virus was not contained in any vaccine used during the pandemic (let alone before it) because we simply did not know that the disease was caused by the virus (or any virus at all). This is where the elaborate lore construction of conspiracists takes hold because it is at this point that they argue that this doesn’t matter because the influenza virus was not in fact the cause of The Mother of All Pandemics, but rather it was bacteria. The trouble is that the historical record shows beyond any reasonable doubt that influenza was the cause of the pandemic- but there is a kernel of truth to this (as is often the case with conspiracy theories).
Autopsy studies showed that influenza in the 1918 pandemic was a major cause of bacterial superinfections to a degree that was not seen in future pandemics (but the general phenomenon of bacterial superinfection continues to be seen with many viruses, including seasonal influenza). This reflects that controlling an influenza pandemic may mean not simply having effective influenza antivirals but effective antibiotics to address the bacterial superinfections- but it doesn’t mean that the pandemic in question was not caused by influenza. Influenza is known to be able to cause bacterial superinfections in the lung through multiple immunological mechanisms, some of which are summarized in the figure below:
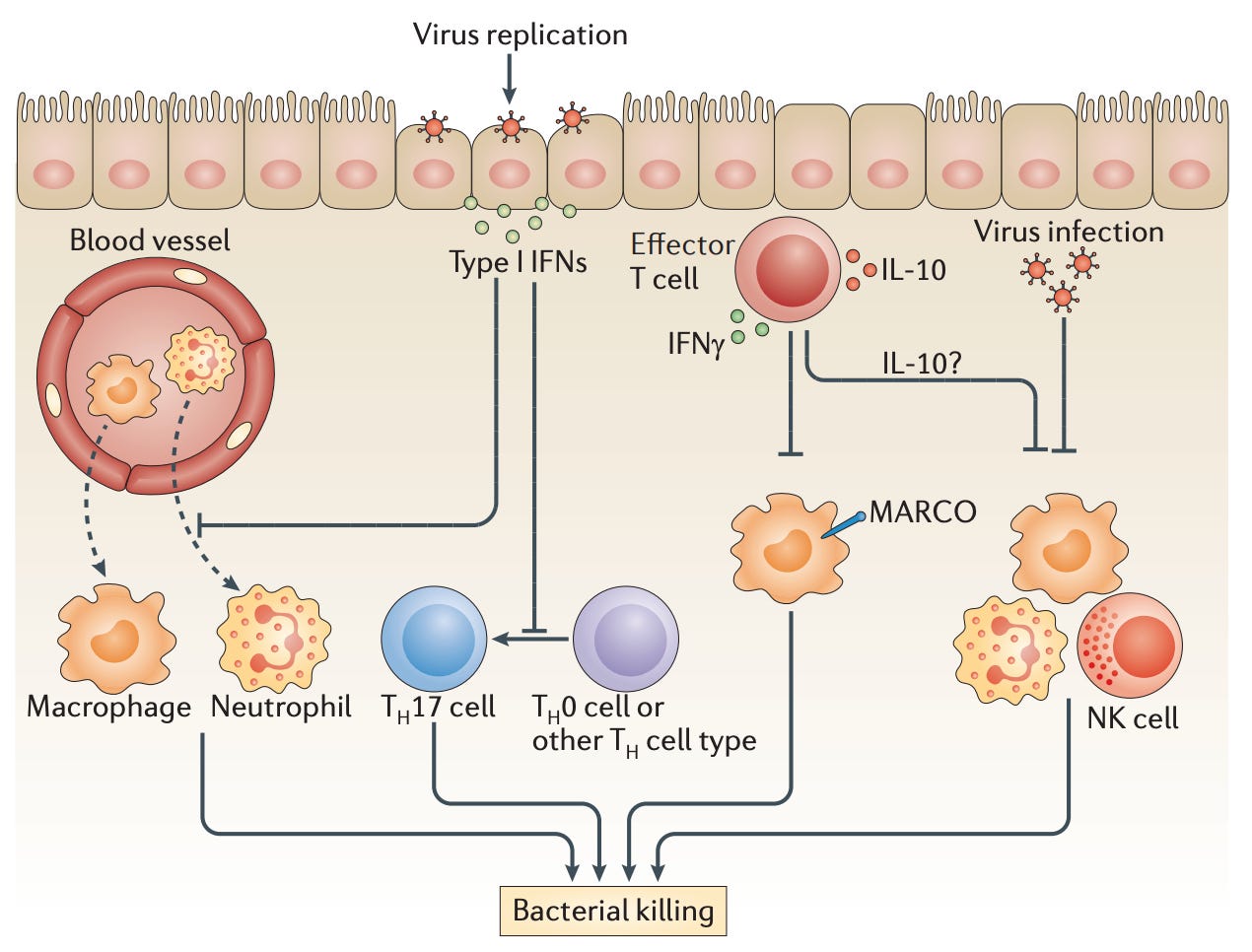
Another aspect to this has to do directly with the virology of influenza: in addition to simply removing epithelial cells (by killing them) and exposing the extracellular matrix therein to allow bacterial invasion, influenza uses a neuraminidase enzyme on its surface to escape from cells it has infected and infect other cells. Neuraminidase removes sialic acids10, and can do this on the extracellular matrix, allowing for binding sites for bacterial proteins to become exposed and facilitating entry into the lower respiratory tract, causing pneumonia. Neuraminidase also triggers the production of an anti-inflammatory cytokine (TGF-beta) which also prevents effective immune responses against microbes. Indeed, influenza substantially increases colonization and carriage of these microbes in children. The bacterial pneumonias seen in the deceased victims of the 1918 pandemic were caused by influenza.
In summary: there is no reasonable possibility that the 1918 influenza pandemic was caused by a vaccine and the evidence is entirely consistent with the pandemic being caused by an influenza A H1N1 virus.
For the record, this is not new ground for Rogan’s podcast- Rogan has literally featured Peter Duesberg on his podcast, an AIDS denialist whose meddling in South African policy caused for a rejection of antiretroviral medication that is estimated to have resulted in 171,000 HIV infections, 330,000 deaths and 35,000 babies born with HIV- a decision that Rogan appears to have no remorse over (it is incorrectly spelled “Duisberg” in the hyperlink) as he explained to Robert Malone when the latter public health menace was on his podcast.
Coincidentally, 1892 is often regarded as the year virology was born as it is when actual viruses were first discovered (they had been hypothesized to exist before this but not shown). Ivanovskii showed that the cause of tobacco mosaic disease could be passed through a filter that excluded bacteria in 1892 and Beijerink subsequently showed in 1898 that the cause of tobacco mosaic disease was replicating in living plant tissue by serial infections of this filtered matter.
Haemophilus influenzae type B (sometimes called Hib) is microbe that causes a devastating vaccine-preventable disease (which is not influenza) and can include manifestations like epiglottitis and meningitis. Other strains of the bacterium can also cause disease in humans but no vaccine is yet available for them and Hib tends to be the most severe by a significant margin.
Pfeiffer struggled greatly to grow the bacillus across multiple media but initially could not get it to persist for more than a single generation (it seemed that other bacteria from the patient samples would outcompete it). Shibasaburo Kitasato, the Japanese physician and bacteriologist who co-discovered the cause of plague and invented diphtheria antitoxin, had been visiting Koch’s laboratory while Pfeiffer had been working on this problem, and was able to come up with a method that grew the bacterium for 10 generations with culture media similar to what Koch had used for culturing Mycobacterium tuberculosis, the cause of tuberculosis. Pfeiffer than had the insight that perhaps the bacteria needed a complex of proteins like those found in patients for efficient growth, at which point he tried to use blood agar. This proved successful, and demonstrated a fundamental principle in microbiology that different bacteria may require different culture conditions to grow effectively. Indeed, the key component to growing the bacillus was actually hemoglobin.
Interestingly, the sheep’s blood that is generally used for blood agar actually interfered with the growth of the bacillus due to an enzyme it contained. Rabbit and human blood however actively supported the infection.
Bacteria are extensively classified by their properties and by how they stain with different dyes. One major example is the Gram stain which measures the peptidoglycan content of the bacterial cell wall with crystal violet dye (or methylene blue) and safranin (which is pink) or fuchsin (which is red) that is then washed away with ethyl alcohol and acetone. Bacteria that stain purple (indicating retention of the dye) are said to be Gram positive. Bacteria that stain pink (indicating the dye is washed away because it can’t stick to the peptidoglycan) are said to be Gram negative. Some bacteria are said to be Gram indeterminate meaning they can stain purple or pink in an unpredictable way (these are sometimes called atypical bacteria) and some bacteria stain both purple and pink (which is known as Gram variable). The significance of this is not just for classification: some antibiotics work only on Gram-positive organisms, while others only work on Gram-negative. Haemophilus influenzae is considered Gram-negative and does stain under methylene blue but will not Gram stain.
David Davis was initially very critical of Pfeiffer’s claims noting that his original papers describing the bacillus were lacking in statistical details (which was correct). Davis decided to conduct an experiment: he took a culture of Pfeiffer’s bacillus and infected himself via his nose and tonsils, at which point he developed a respiratory illness consistent with influenza and continued to have culturable bacilli for over a month. However, other investigators found problems in Pfeiffer’s work. In one study, only a minority of patients with influenza were found to have Pfeiffer’s bacillus but almost all whooping cough patients were. The bacillus was also found in the throats of a number of other illnesses like chickenpox, meningitis, tuberculosis, measles, etc. which led to the perspective that Pfeiffer’s bacillus was actually a “saprophyte,” which today would be properly known as a pathobiont- a microbe that is a normal component of our own flora that has the potential to cause disease under some conditions but is not uniformly pathogenic, which we know to be correct today.
Viruses are defined by the fact that they will not grow on their own: they require the presence of cells that are both permissive (meaning they express a receptor that allows viruses to enter them) and susceptible (meaning their metabolism is able to support replication of the virus) for replication. Some filterable agents could be supported solely with bacterial growth media, like mycoplasma. Hence the term “filterable agent” and “virus” are not synonyms, though they are related.
Avian (H5 and H7) influenzas have a furin (polybasic/multibasic) cleavage site which exposes the fusion peptide. Other influenzas instead have a tryptic (monobasic) cleavage site.
More recently, it has been shown that pneumococcal vaccines (against Streptococcus pneumoniae) are protective against non-bacteremic bacterial pneumonias associated with influenza. It is not entirely clear why the prior vaccines used in the 1918 pandemic did not appear to have efficacy, but may be related to the specific endpoints chosen to measure the effectiveness of the vaccines (i.e. you would only see a benefit when looking at pneumonia, not influenza-like illness broadly).
Influenza entry is governed by its hemagglutinin protein which binds sialic acids on the surface of cells to eventually enter them by the endocytic pathway. Once there, the hemagglutinin protein is processed by cellular enzymes and the virus is able to enter the cells and replicate. However, there is a problem- on the way out of the cell to infect new cells, influenza hemagglutinin will still stick to sialic acids on the surface of the cell. To effectively escape, the neuraminidase enzyme will cleave sialic acids from the cell surface. This means that antibodies that block the action of neuraminidase have a neutralizing effect. It also means that for influenza to be an effective virus requires a delicate balance between the function of both hemagglutinin and neuraminidase. A neuraminidase that is too fast can destroy influenza receptors before the virus can enter cells. A neuraminidase that is too slow will prevent influenza from escaping to cause infections in new cells.





